Living or Working Abroad? What do People Think About Us? Find Here All You Need to Know. All the information you need to properly process prescription claims with Cigna.
NeedyMeds - An online information resource of programs that provide assistance to people who are unable to afford their medications and health care costs. Driven by our focus on whole person health, we are delivering even more connected capabilities and innovative solutions that drive savings, engagement, and maximize the value of total health care services. UnitedHealthcare and OptumRx contributed nothing for the drug and then collected the additional $38.
HMO, dental HMO, and other. Search, compare and save. So now, portions of your policy premiums can go to not one but two buy back programs…a two fer. Optum is committed to providing the best health services, leading the way to better experiences, better health and lowers costs for you. Cigna HealthCare of Illinois, Inc.
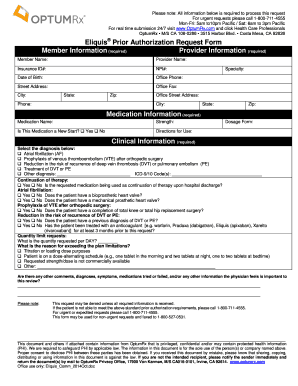
Brand and generic options are included in the broad list of covered prescription medications. Other ways to submit prior authorization forms. PRESCRIPTION REIMBURSEMENT REQUEST FORM Use this form to request reimbursement for covered medications purchased at retail cost.
Complete one form per member. Additional information and instructions on back, please read carefully. Member Information RxGroup (see ID card) Member ID (see ID card) Last Name.
The OptumRx Health Care Professionals Portal is a one-stop source for those who write and fill prescriptions. Connecting billions of data points, we empower doctors to make informed decisions. We tackle trends and pinpoint solutions for our clients. And we work every day to simplify the system. Optum is applying innovative technologies to the business of health care and is incorporating health care expertise into technological innovations – as a result, creating partnerships across the entire health care ecosystem, making it work better for everyone.
It also reinforces the role that pharmacy benefit management (PBM) plays in the drug channel. Before you get starte in addition to your insurance car you will need the following information. This information can be obtained by contacting your prescribing physician. The OptumRX Prior Authorization Request Form is a simple form to be filled out by the prescriber that requests that a certain treatment or medication be covered for a patient.
A list of tried and failed medication must be provided as a justification for the request alongside the diagnosis. OptumRx has partnered with CoverMyMeds to receive prior authorization requests, saving you time and often delivering real-time determinations. The big question: Will patients benefit, or will this just protect insurance. For example, if a drug costs $3.
UnitedHealth Group already owns OptumRx , a fast-growing PBM and CVS Health, which owns the Caremark PBM,. For assistance, please call the number on the back of your debit card. AARP Prescription Discounts provided by OptumRx (Program) is a prescription drug program that provides a discount on FDA-approved drugs that are not covered by an insurance plan or Medicare prescription drug (Medicare Part D) plan.

The Program, endorsed by AARP , is administered by OptumRx Discount Card Services, LLC.
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.